Overview
Human T-lymphotropic virus type 1 (HTLV-1) is an oncogenic retrovirus (a virus that can cause cancer), that causes a chronic infection affecting CD4+ T-cells. There are no proven associations between viral subtype and transmission patterns or health outcomes. There are very limited data about transmission patterns and health outcomes in Australia however research is currently being undertaken.
HTLV-1 Sub-Types
There are seven main subtypes (A to G) worldwide, the subtype A occurs globally, subtypes B, D, E, F and G are found in Africa and subtype C in Australia and Melanesia. Countries with HTLV-1c subtype include Papua New Guinea, Solomon Islands, French Territory of New Caledonia and Vanuatu.
There is a significant lack of data that is specific to Central Australia or subtype C, this includes but is not limited to transmission routes and risk factors, impacts of breastfeeding and HTLV-1 infection, rates of HTLV-1 associated conditions and possible disease associations to HTLV-1 infection. While there is more data known about other subtypes and in other populations the technical report by WHO describes a global lack of systemically collected information around prevalence and particularly for HTLV-1-related diseases. These guidelines are written using what is known internationally and locally, recognising the paucity of knowledge as described.
Epidemiology
WHO estimates 5–12 million people are infected with HTLV-1 globally. HTLV-1 prevalence is poorly understood but is known to be extremely variable, often characterised by discrete geographical areas of higher prevalence. Countries and regions considered to have areas with endemic HTLV-1 include Japan, the Islamic Republic of Iran, Australia, Latin America, the Caribbean, Melanesia and West Africa. Prevalence generally increases with age and is higher in females than males.
There is limited information about the Australia wide-prevalence of HTLV-1. Overall, the prevalence of HTLV-1 in the general population is extremely low. Blood donor surveillance data from 2013–2022 found a prevalence of 4.4 per 100,000 donations with no significant trend over the period. Most (85%) positive donors were born outside Australia.
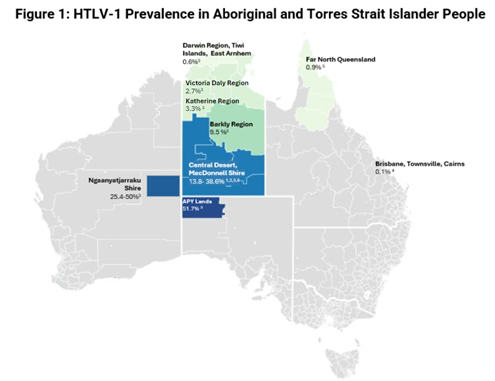
HTLV-1 Epidemiology in Aboriginal Communities
In some remote Aboriginal communities, the prevalence of HTLV-1 is high (Figure 1). The prevalence of HTLV-1 is highly variable across geographic regions and populations in Central Australia. Two large community-based studies have been conducted in Aboriginal communities in the Alice Springs region. The first study assessed HTLV-1 prevalence and transmission risk factors, revealing infection rates of 3.5% in children under 15 and 36.8% in adults. Prevalence increased with age, reaching 49.3% in individuals over 45 in that cohort. The second study examined the association between HTLV-1 infection and noncommunicable diseases, finding a prevalence of 38.6%.
There are no data specific to young children. However, one community-based study reported prevalence by age and sex. The prevalence in children aged under 15 years was 4.3%. Prevalence increased markedly with age suggesting transmission between adults account for the bulk of cases, consistent with other countries.
The sex-distribution within Central Australian Aboriginal communities is markedly different from many other HTLV-1 affected populations, with higher rates observed among males. This atypical sex distribution may indicate non-sexual transmission, such as blood exposure, may play a role.
The community-based studies have reported higher prevalence in Central Australia communities, particularly in areas to the South and West of Alice Springs. A laboratory-based study found relatively high prevalences in people living in areas adjacent to Central Australia including the Aṉangu Pitjantjatjara Yankunytjatjara (APY) lands of South Australia (51%), Barkly (9.5%), Katherine (3.3%) and Daly (2.7%) regions. There was a low prevalence in Darwin (0.6%), which is consistent with another study of children with bronchiectasis in Royal Darwin Hospital. An older community-based study from the West Kimberley found a prevalence of 15%, however methodological and reporting concerns limit the certainty of this evidence and further research is needed in this region to determine HTLV-1 prevalence. A large seroprevalence study in Queensland found HTLV-1 prevalence to be 0.1%.
Areas with High HTLV-1 Prevalence in Australia
There is no globally accepted definition of “high prevalence”. The European Centre for Disease Prevention and Control consider above 1% in the general population to indicate high prevalence. The prevalence in pregnant women in the three countries recommending routine antenatal screening is 0.26-1.05%.
These Guidelines define the following region as having high HTLV-1 prevalence, as demonstrated through multiple published studies:
- Central Australian region including:
- Central Australian region in the Northern Territory
- Aṉangu Pitjantjatjara Yankunytjatjara (APY) lands in South Australia
- Ngaanyatjarra (Ng) lands in Western Australia
These Guidelines also define the following regions as being likely to have high HTLV-1 prevalence, although the strength of this evidence is weaker:
- Barkly region of the Northern Territory (based on 31 positive results)
- Katherine region of the Northern Territory (based on six positive results)
- Daly region of the Northern Territory (based on two positive results)
These regions and documented prevalences are outlined in Figure 1:
Recommendations in these Guidelines relate to communities in all four regions. People residing in adjacent areas, or who have connections to high prevalence areas but are no longer residing there, may also have high pre-test probability and could be considered for testing if considered appropriate by treating clinicians.